How to Think about the Drug Crisis
Almost nobody is taking America's drug crisis seriously. To be sure, the ever-mounting deaths attract headlines. They get a mention in the State of the Union, or on the campaign trail. But based on the outcomes, policymakers appear to have more or less given up.
Some numbers put the problem in perspective. After Covid-19, drugs are now the leading driver of America's steadily declining life expectancy. A reported 111,219 Americans died from a drug overdose in 2021. That figure has risen more or less unabated, and at an increasing pace, since the early 1990s. Back in 2011, 43,544 Americans died from a drug overdose — less than half the 2021 figure. Ten years earlier, in 2001, it was 21,705 — less than half as many again. And the problem keeps getting worse: The 2021 figure is nearly 50% higher than it was in 2019.
Compared to the scale of the problem, our ambitions to meet it are meager. In its 2022 National Drug Control Strategy, the Biden administration set a goal of reducing overdose deaths by 13% over the next two years. That would still mean 83,000 overdose deaths annually — higher than any year before 2020. Thus far, the trajectory is not positive: The National Center for Health Statistics estimates that there were roughly 110,000 overdose deaths in the year ending December 2022 — essentially unchanged from a year earlier.
Of course, President Biden is not uniquely to blame. Overdose deaths rose through the Obama and Trump administrations; the seeds of the crisis were planted as far back as Bill Clinton's first term. The failure has been ongoing and systematic. It is in part a failure of know-how: Over a century into drug control, we still have only limited ideas about how to abate the harms of drugs. It is also a failure of knowledge. One can easily find out how many people died of Covid-19 last week, but we still have only estimates of how many people died of drug overdoses last year. And of course, it is in part a failure of political will.
But in crucial respects what we face is a failure of understanding. What many people — policymakers and the general public alike — fail to grasp is that today's crisis is not like crises past. Historically, drug crises were characterized by the (re)emergence of a drug, followed by the spread of addiction and its attendant ills. The problems they caused affected individual and social health — physical illness, social dysfunction, frayed relationships, public disorder, etc. While these still play a role, today's crisis is predominantly characterized by an unprecedented increase in the drug supply's lethality. Historical crises inflicted many more or less equally weighty harms — to users' health, to families, to communities. In this crisis, one problem dwarfs all others: death.
Drugs have changed, probably for good. They now kill their users. Until policymakers internalize this fact, they will not make any progress. A haphazard approach was tolerable when the harms of drug use took time to accumulate. But with tens of thousands being poisoned to death every year, bolder action is required.
THE NEW DRUGS
Humans have long used drugs, to the benefit of some and the detriment of others. But drug crises — society-scale problems caused by drugs — are a relatively recent phenomenon.
The first true drug crisis in American history did not occur until after the Civil War, when tens of thousands of soldiers received morphine via hypodermic needles — both recently invented — and brought the subsequent addictions home with them. In the half-century between that crisis and the first wave of national drug-control legislation, thousands more became addicted. The opiate epidemic did eventually decline, before emerging again in a different form in the late 20th century.
These early drug crises were crises of addiction and its attendant harms, to the user and to those around him. The various postwar drugs of abuse — Benzedrine, for example, and barbiturates — were controlled because they led to undesirable dependency and harmful misbehavior. Similarly, the thousands of soldiers who returned from Vietnam addicted to heroin were a cause for concern, both for the effects of chronic opioid use on users' health and for the social harms of homelessness and other dysfunctions attending that use. The crack crisis of the 1980s added a wrinkle, insofar as the drug's sale was associated with particularly violent gang crime. But even then, the problem was the harmful side effects of compulsive drug use. It was not, first and foremost, the fact that drugs killed people.
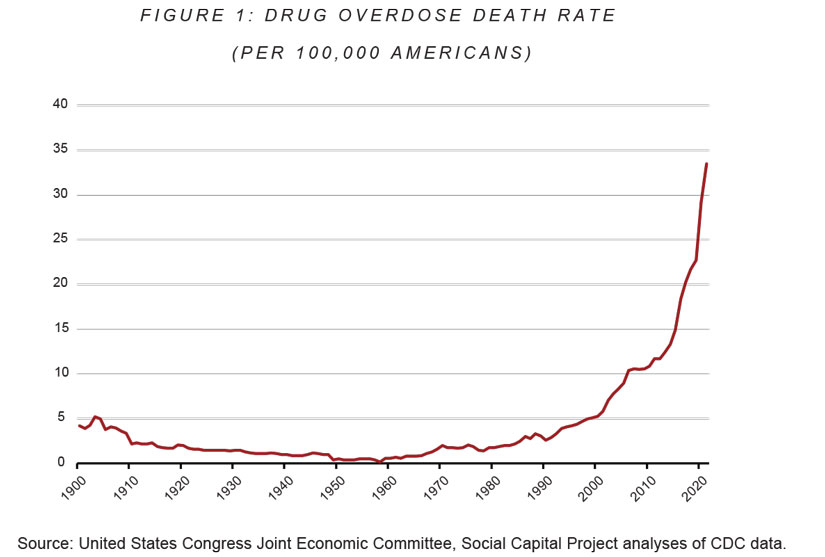
This is not to say that drugs did not kill people in the past; they certainly did. But compared to other causes of death, drug overdose was uncommon. Between the end of World War II and 1966, data compiled by the Social Capital Project of Congress's Joint Economic Committee indicate that less than one in 100,000 Americans died from drug overdoses annually. As drug use grew more common, overdose death rates rose slightly. But even in the late 1980s — the height of the crack crisis — only about three in 100,000 Americans died from a drug overdose per year. In 1988, the peak year for drug overdose in the '80s, Americans were roughly three times more likely to die by homicide, four times more likely to die by suicide, and six times more likely to die in a car accident than by overdose.
In the mid-1990s, something changed. Death rates began rising, slowly but exponentially. Between 1990 and 2000, the overdose death rate doubled, from 2.6 per 100,000 to 5.3 per 100,000. The decade between 2000 and 2010 saw another doubling. From 2010 to 2020, the rate tripled, to 29.2 per 100,000 — 10 times the rate in the 1980s, and 30 times the lows of the postwar period.
Drug overdose is now the leading cause of non-medical death in the United States. As of 2021, it was only slightly less deadly than all homicides, suicides, and motor-vehicle fatalities combined. Drugs still cause addiction, of course, and addiction still hurts addicts and society. But, likely for the first time ever, the primary harm of today's drug crisis is death.
DRUG INNOVATION AND DEATH
At the most abstract level, two changes explain this increase. The first is that the number of people using drugs has risen somewhat. The second is that the death risk of drug use has increased exponentially.
The story of the first change is relatively well known. As the American Enterprise Institute's Sally Satel has documented in these pages, in the early 1990s, physicians began prescribing more opioid painkillers at much higher doses. Many people became addicted, either to something they were prescribed or to pills diverted from the expanded legal supply. The growth of the drug-using population — and therefore the overdose risk — surely explains some of the increase in overdose deaths.
But a growing number of users cannot fully explain that increase. Estimates from the RAND Corporation indicate that between 2006 and 2016, the number of chronic heroin and methamphetamine users rose about 40%, while the number of chronic cocaine users fell 40%. In the same period, cocaine-involved deaths rose 30%, meth-involved deaths rose 380%, and heroin-involved deaths rose a staggering 617%. There are not just more people using drugs; drugs are killing more people.
Historically, illicit drugs — heroin, cocaine, marijuana, etc. — were derived from plants grown in fields or greenhouses. But licit pharmacology has long been able to use simple, widely available precursor chemicals to synthesize the active ingredients in these substances. This sidesteps the complex processes of farming altogether. At some point in the past several decades, drug-trafficking organizations learned to use the same techniques at scale. Using precursors sourced primarily from China, they now synthesize a variety of opioids — the class of drugs that includes heroin.
The most widely known of these is fentanyl, a synthetic opioid conventionally used in anesthesia that is 50 times stronger than heroin. Some are stronger still — carfentanil, the most potent opioid known thus far, is roughly 100 times stronger than fentanyl. In 2021, synthetic opioids were involved in roughly two out of every three overdose deaths.
The problem is not just fentanyl, though; it's the fact that a wide variety of drugs — many of which are visually interchangeable white powders — are now adulterated with fentanyl. In many places, most "heroin" sold on the street is really fentanyl. Many cocaine overdose deaths now involve synthetic opioids, as fentanyl is added to or sold as cocaine. Pills sold as a variety of substances are often just pressed fentanyl. Particularly dangerous is the combination of synthetic opioids with benzodiazepines, which amplify one another's depressant effects and further drive up the risk of overdose and death.
Complicating the story further is the increasing purity and declining cost of methamphetamine, another synthetic drug with an exploding death rate. After synthetic opioids, methamphetamine is now the second most common cause of drug overdose death. It's also the only tracked drug where deaths not involving synthetic opioids are increasing. That these two lab-produced substances are replacing "organic" drugs at the same time is not a coincidence.
Why have these drugs taken over the market? Because they're a much better value proposition for sellers. Synthetic drugs significantly reduce production costs, both because chemistry is less labor- and input-intensive per unit produced than farming and because lab production is much easier to obscure from interdiction efforts that drive up costs. Furthermore, because the potency per dose is higher, drug-smuggling operations can move a smaller amount of fentanyl than heroin for the same profit.
Of course, the stronger the drug, the higher the risk of overdose. Drug-overdose death rates used to be low in part because for the first century or so of modern American drug use, the potency of illicit drugs was constrained by what traffickers could grow in a field. Synthetic drugs remove this limit.
Stronger, cheaper to make, and easier to hide from law enforcement: It's no wonder synthetic drugs are rapidly crowding their non-synthetic counterparts out of the market. Seen in this light, the exponential growth curve of deaths is just a byproduct of exponential productivity growth in a rapidly innovating industry.
DEATH IS DIFFERENT
The emergence of synthetics has altered the balance of the harms associated with drug use. While addiction is still an issue, death now constitutes a far larger share of the problem. This has significant implications for the mitigation strategies the situation demands.
Drug addiction and its harms tend to grow over the number of use sessions. A relatively large proportion of people who try drugs, even seriously addictive drugs like heroin, only use once or twice, and do not end up addicted. Among those who use compulsively, the physical effects of addiction don't manifest immediately: Organs are stressed, veins go bad, psychological symptoms develop, and hair and teeth fall out over time. Social harms often take time to compound, too — alienating friends to pursue a high usually manifests after months or years of abuse, as does deteriorating performance at work. Such problems also concentrate in the most heavy and compulsive users.
Death is different. The risk of overdose death is not uncorrelated from history of use; both tolerance and probability of more aggressive use rise with time. But that risk exists in any use session. Death is an all-or-nothing proposition: Either this dose kills you, or it doesn't. Whereas historically, most of addiction's harms were concentrated among the population of the most serious users, a more deadly drug supply means that the risk that any given use session results in death is much higher.
In decades past, educators illustrating the harms of drug use usually described a life course: Someone tries a drug and gets hooked; he uses compulsively, burning through money and friends; and eventually he hits "rock bottom" or, in some cases, dies. Today, these events can all still happen. But the risk of death is also much, much higher, and can occur at any point along the life course of drug use.
Drug control has long posed a thorny dilemma for policymakers. Drugs undoubtedly impose substantial social and individual costs. But enforcing prohibition and providing treatment also impose costs — in time, money, and in some cases, liberty.
Proponents of drug legalization have long argued that the cure of prohibition is worse than the disease. More careful analysts of the situation have still tended to view "cure" costs as substantial and not always and everywhere justifiable. At certain margins this implies drug use can be tolerated, because the costs outweigh the benefits of deterring it.
Today's drug crisis, however, dramatically alters the balance of costs and benefits. Loss of life dwarfs all of the other costs imposed by drug use, on both the individual and society. As a consequence, the level of drug use that can be tolerated drops, particularly for those drugs that are most likely to lead to death. This means the amount of time and energy the government dedicates to the mitigation of drug use and addiction must increase substantially.
DEALING WITH DEATH
Given that today's drug crisis is fundamentally different from drug crises past, different policy measures are required to address it. Some dramatic shift is needed along at least some margin. But where should policymakers concentrate their attention and resources?
One increasingly common answer is "harm reduction," the umbrella term for interventions meant to reduce the harms associated with drug use short of encouraging cessation. Harm-reduction programs — distributing naloxone, operating needle exchanges, or setting up safe consumption sites (SCSs) where people can use under supervision — are gaining increased traction as a solution to the rise in deaths. Major urban areas from New York City to San Francisco are investigating or embracing harm reduction; the Biden administration has handed out tens of millions of dollars in harm-reduction grants.
Proponents argue that harm-reduction strategies are particularly well suited to the current crisis. The drug supply is toxic, they argue, so policymakers should prioritize reducing its toxicity over controlling its use. Opponents of harm reduction, meanwhile, often frame their objections in moral terms — we shouldn't facilitate drug use and addiction, even toward some instrumental end. But the "death is different" view provides another critique: Harm-reduction strategies are a poor fit for the current crisis because they address the safety of individual use sessions rather than trying to discourage people from using altogether. Such approaches may help to address accumulating harms, but they are not well suited to a risk that obtains across all use sessions and for which a single failure results in death.
Indeed, the evidence suggests harm-reduction interventions have a limited impact on death rates. As of 2021, according to three prominent drug researchers, "existing literature on naloxone access laws," which increase the availability of naloxone, "provides inconclusive evidence for reduced fatal opioid overdose." Of the two quasi-experimental studies on SCSs' effect on overdose death rates — one in Sydney, the other in Vancouver — the first finds no significant impact, while the other finds a reduction only in the site's immediate vicinity. This may be because SCSs keep users safer when they use at the sites, but they do little to affect whether they are using at all, thus extending their lifetime of use and, in turn, their probability of death. This may also be the case for needle exchanges: Recent quasi-experimental evidence finds that while such exchanges reduce HIV infection, they also increase rates of opioid-overdose hospitalization and death.
The point here is not that governments should not hand out naloxone — they should, because each overdose prevented is good in and of itself. But when every use session carries the risk of death, we should not expect per-use session interventions to have a dramatic impact on death rates.
Instead, policymakers need to prioritize the most efficient route to minimizing lifetime overdose risk: stopping people from using altogether. This, of course, is not a new idea. But to build a policy at scale to address the current crisis, policymakers need to emphasize efforts on this front like never before. In particular, any successful policy must speak distinctly to the needs of the two groups now at risk of overdose deaths: the most compulsive problem users, and everyone else. The interventions necessary to address each population's risk of drug use — and therefore drug death — are different.
PROBLEM USERS
A rule of thumb is that for any addictive substance — legal or illegal — consumption is power-law distributed. That is, 20% (or less) of the users consume 80% (or more) of the substance. The former are also the users among whom problems are most common, including most likely deaths. For this population — those who not only use, but are seriously, actively addicted — the best tool available is treatment. A proportional policy response to these individuals' needs must focus on offering — and compelling — treatment like never before.
How many Americans need treatment? As of 2020, survey data suggest that roughly 18 million Americans had in the past year suffered from an illicit drug-use disorder, including 4.2 million whose disorder involved a drug other than marijuana. Just 2.6 million people, however, reported actually receiving treatment that year, including 800,000 who received medication-assisted treatment (MAT). The survey from which those estimates come, the National Survey on Drug Use and Health (NSDUH), likely underestimates the true prevalence of abuse: One study that attempted to account for insufficiencies in the NSDUH found that more than 7.6 million Americans suffered from an opioid-use disorder, while only about 1 million were receiving MAT.
No matter how one counts, these results represent a substantial "treatment gap" for substance abuse. Millions of Americans who should be in treatment are not; millions more may be in treatment but without access to medication to facilitate their recovery. This was bad enough when drug use was a problem of addiction. But in the current crisis, each day an addict spends out of treatment is a day he may overdose and die.
To be sure, treatment is far from perfect: The National Institute on Drug Abuse estimates that relapse rates from treatment are between 40% and 60% — on par with recurrence rates for hypertension and asthma. But it is also the least-worst tool we have to stop use among people with addictions. Filling the treatment gap is therefore the most important step we can take to address the crisis.
For disorders responsive to it, MAT is considered the gold standard of substance-use-disorder treatment. In the case of opioid-use disorder, we have three FDA-approved treatments available: methadone, buprenorphine, and naltrexone. While they operate using different mechanisms and have different drawbacks, broadly speaking each works by binding to the brain's opioid receptors, calming cravings and substituting for addictive opioids without inducing the same harmful side effects. MAT has been shown to substantially improve outcomes when compared to a placebo and to psychological therapy alone.
There are, of course, risks associated with such treatments. Several thousand people die every year from methadone toxicity, likely using methadone diverted from the clinic system. This is a reason to prefer buprenorphine, which has been shown to have a lower potential for abuse and harmful side effects. It is also a reason to prefer abuse-resistant formulations like suboxone (a combination of buprenorphine and naloxone) and once-monthly injectable naltrexone. There are also those who contend that MAT entails the substitution of one addiction for another. On some abstract philosophical level this is true, but it is akin to, say, replacing an addiction to cigarettes with an addiction to coffee — both are used compulsively, but one kills far less often than the other.
Even granting the risks, at current margins the United States uses too little MAT, not too much. Roughly three in four Americans who could benefit from MAT do not use it. As of 2020, only about half of drug-treatment facilities surveyed by the Substance Abuse and Mental Health Services Administration (SAMHSA) provided any MAT. Meanwhile, 20% of opioid-treatment-program facilities did not provide buprenorphine, and 60% did not provide injectable naltrexone.
How can policymakers expand access to MAT? Congress took a major step forward in its last spending bill, ending the long-standing requirement that physicians receive a special waiver to prescribe buprenorphine. Previously, only about 5% of physicians were licensed to do so. But some clinicians have warned that simply ending the "X Waiver" will not be enough, as access to MAT is still limited in areas with low prescribing capacity.
One way to address these concerns is to continue the relaxed restrictions on prescribing buprenorphine via telemedicine adopted during the pandemic era. Concerns about increased diversion under relaxed prescribing rules are legitimate, but given adequate oversight, the benefits of increased access to MAT will likely outweigh the potential costs.
Other commonly cited approaches to expanding MAT access include increasing its availability in prison, jails, and community-supervision programs, where it is systematically underused. According to the state policy news outlet Stateline, as of 2018, only one state — Rhode Island — offered all three FDA-approved medications to its inmates. As of 2019, just 36% of people on parole and 31% of those on probation with an opioid-use disorder received MAT.
Psychotherapy is always recommended in coordination with MAT. It is also the first line of defense for substances for which there is no MAT, like cocaine or methamphetamine. Therapists have various evidence-based treatment approaches available, including cognitive behavioral therapy, 12-step facilitation, and contingency management. This last method — which involves paying patients small amounts of money for staying clean — is controversial. But it appears to be comparatively more effective for treating stimulant use in particular, which is important given the lack of MATs for these substances. The Biden administration has authorized a limited expansion of the amount contingency-management programs can pay clients. While this innovation should be closely watched, it may provide a framework for future interventions — especially those aimed at stemming the rising methamphetamine deaths.
Regardless of the type of therapy offered, facilities are currently suffering from a dearth of inpatient treatment beds. Facilities responding to SAMHSA's 2020 survey reported that roughly 80% of their beds were currently in use. Insofar as the federal, state, and local governments all provide inpatient facilities, they can expand availability in public facilities directly. They can also coordinate between treatment providers to help fill unused spots with people in need. A substantial investment in both public and private treatment is almost certainly required to ensure enough beds are available for everyone who should have one.
Increasing the availability of treatment, however, can only go so far. The treatment gap is not merely a product of the supply of treatment, but also of the demand for it. As Stanford addiction specialist Keith Humphreys has argued, while addiction is a disease, it differs from other diseases in that its symptoms entail "intense neurological reward." As a result, many people do not enter treatment because the incentives to continue using outweigh the incentives to quit. In many cases, then, the best way to help people is to compel them into treatment.
Compulsory treatment is controversial, with critics arguing that treatment is less likely to work if the patient does not want to change. But the balance of the evidence, as indicated by a nine-study systematic review, suggests that outcomes in compulsory treatment are similar to those of voluntary treatment. What's more, compulsory treatment will reach patients that voluntary treatment will not. If the goal is to increase treatment use, we must significantly expand compulsory treatment.
The most obvious area for expanding compulsory treatment is within the criminal-justice system. Estimates suggest that between a quarter and a third of people with a heroin-use disorder pass through correctional facilities every year, while 17% of state prison inmates and 19% of jail inmates regularly use opioids. Drug use is implicated not only in drug-possession offenses, but also in property and violent offenses, meaning that individuals entering the criminal-justice system for a variety of reasons may benefit from treatment. Yet many do not receive it: Based on one estimate, less than a fifth of those in need do.
At the very least, state and local jail, prison, and community-supervision administrators must prioritize the availability of FDA-approved MAT for their charges, along with continued access and care following reentry — particularly in probation and parole programs. But states can go further. For instance, jail inmates can be diverted into drug-court programs that offer a suspended sentence in exchange for compliance with treatment. Such programs have been shown to significantly reduce recidivism. Additionally, given the criminal-justice system's outsized role in effective treatment, policymakers should think twice before decriminalizing small possession, as the state of Oregon has. If police cannot arrest users, they cannot divert them into treatment.
The other coercive mechanism for treatment is civil commitment. This entails a court ordering individuals into either inpatient or outpatient treatment based on a showing that they are a threat to themselves or others. Thirty-eight states authorize civil commitment for substance-use disorder, but according to a 2017 report, the laws remain "seldom used." Many states have revised such laws in recent years; others should follow suit.
Without evidence-informed MAT, civil commitment is unlikely to benefit patients, and may even harm them. But for individuals outside the criminal-justice system who suffer from addiction and are a danger to themselves and others, it must be a component of the treatment-gap-filling strategy. While some civil libertarians disdain civil commitment as an unmerited deprivation of rights, people with substance-use disorders often see the sense of the strategy: A survey of 250 people in inpatient opioid-detoxification programs found that, on average, they supported civil commitment for drug use and psychiatric disorder.
At the very least, states should provide information to families about the use of civil commitment more proactively. States wishing to go further can also make civil commitment proceedings a broader component of their public-health strategy. After all, rising overdose death rates change the calculus around civil commitment. In the past, lawmakers had to weigh the interest of liberty against the interest of health — was addiction bad enough to merit depriving someone of his freedom? Now, they must weigh the interest of liberty against the interest of life — and there is a far stronger case for depriving someone of his liberty to stop him from poisoning himself to death than to protect his health. Ensuring that parents or doctors seek civil commitment for their addicted but treatment-resistant child or patient, and are informed about the procedure to do so, will almost certainly save lives.
Building the treatment capacity necessary to address the current crisis will involve concessions from both sides. Conservatives will need to get more comfortable with opioid-replacement therapies, with experimenting with treatment approaches like contingency management, and with expansively funding treatment. Liberals, meanwhile, will need to accept that the criminal-justice system has a role to play in treatment, and that sometimes people need to be compelled to get clean. But such concessions are necessary — hundreds of thousands of lives are on the line.
EVERYONE ELSE
Late last year, the Wall Street Journal reported on three high-status casual drug users — an investment banker, a lawyer, and a social worker — who ordered cocaine from the same New York delivery service. The drugs were laced with fentanyl; all three died.
Such stories — of overdose death among people who are not the conventional "faces of addiction" — have grown increasingly common. In one regard, they represent the media's unfortunate preference for more "sympathetic" victims. But they also represent the fact that the harms of drug use are no longer primarily restricted to people who use chronically and compulsively. While people with active addictions will always account for the lion's share of deaths — after all, they account for the lion's share of use sessions — the shift to synthetics means that infrequent users are also at an elevated risk of overdose death. It also means that the risk of even trying drugs has risen — a one-time use carries a far higher risk of death than it did historically.
One conventional way to reduce initiation and drug use is through law enforcement. Supply-reduction operations — everything from busting street dealers to shutting down cartels — reduce the availability of drugs, making it harder for would-be users to use and driving up the price, thereby reducing the number of doses a person with a given amount to spend on drugs can consume. That drugs are illegal, and that those laws are enforced, is almost certainly a significant reason why the prevalence of illicit drug use and addiction is as low as it is. However, rates of enforcement have declined in recent years: The number of drug possession and sales arrests reported to the FBI fell roughly 30% in 2020, and drug-related incarceration has steadily declined for over a decade. All else being equal, we should assume this pullback has contributed to the current crisis.
That said, it would take a substantial investment in this domain to generate an appreciable impact. The shift to synthetics has put law enforcement at a distinct disadvantage by dramatically reducing drug prices — recent estimates suggest that fentanyl prices have fallen rapidly, by roughly 50% from 2016 to 2021. It has also made it much harder to detect and therefore interdict drugs. A great deal more law enforcement is therefore needed simply to return to the pre-synthetic level of efficacy. This would come at substantial opportunity cost to other enforcement priorities, including addressing the recent surge in homicide rates. This does not mean we should forego drug enforcement, as some advocate, or that there aren't law-enforcement strategies that can help. But a huge investment in law enforcement is unlikely to be the silver bullet.
That leaves forms of prevention not involving law enforcement — namely programming aimed at convincing people, especially children, to avoid drugs. Such persuasion is easier said than done; the late drug policy guru Mark Kleiman once derogatorily compared drug prevention to "the Tooth Fairy." Many readers will no doubt recall the heavy-handed public-education campaigns of the 1980s, which seem to have had little impact on drug use. But there is reason to be optimistic about prevention today, if for no other reason than that the current crisis is different. Convincing people of the harms of drug use in the past has been hard, in part because it involves long-term thinking of the sort many people have trouble with. It is plausibly easier to convince people that trying drugs once could kill them — particularly when this fact is demonstrably true.
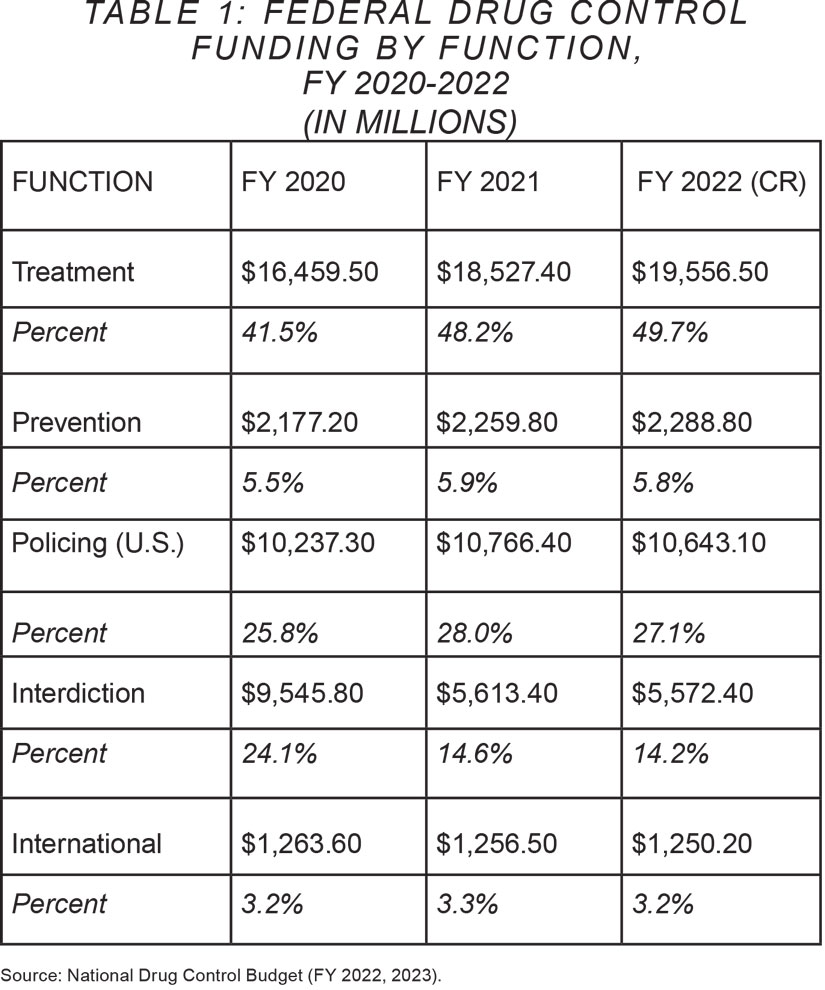
Fiscally speaking, prevention programming is not a high priority among policymakers. The table below breaks down the percentage of federal funding devoted to each type of drug-control method, from fiscal year 2020 to 2022.
As the table indicates, the federal government spent roughly $2.3 billion on prevention during the fiscal year 2022, compared to $19.5 billion on treatment. While $20 billion on treatment is appropriate to the scale of the problem — perhaps even insufficient — spending roughly $50 per American schoolchild does not seem like an adequate commitment to deterring drug use. This is particularly the case because, even under modest assumptions of efficacy, program-based prevention is cheap enough that it handily passes cost/benefit assessments. If nothing else, spending more on prevention is a no-brainer.
What should prevention look like in practice? One common form is the public-education campaign. These have a mixed track record: A 2015 Cochrane Systematic Review identified 14 campaigns, of which eight had no effect, four reduced drug use, and two increased it. But there have been successes, including the Office of National Drug Control Policy's "Above the Influence" campaign and the "truth" campaign, the latter of which has been credited with dramatically reducing teen smoking rates. And we can make some educated guesses about why some campaigns succeed and some fail. One survey of 3,600 school-age students finds that they were more likely to rate as effective anti-drug ads that they also labeled realistic and educational. Researchers tend to argue that when campaigns increase drug use, it is likely because they prime kids to be curious about drugs.
Public-service announcements, including the truth campaign's opioids initiative, have attempted to address the opioid epidemic. Preliminary research suggests that this campaign increased young adults' awareness of opioids generally. But public education about synthetic adulteration has moved far more slowly than the crisis, and in some places has focused primarily on harm-reducing behaviors to the exclusion of pro-abstinence messaging. A dramatic investment in prevention should start with a nationwide educational campaign about how drugs have changed. It should be "realistic and educational," not only because these programs tend to be relatively effective, but because the facts themselves are scary. Too few Americans understand the current problem; we need to address this lack of knowledge.
More targeted prevention programming generally involves teaching young adults about drugs, addiction, and skills associated with resisting the former. Modern prevention programming often focuses on the last of these, attempting to not just educate young people about drugs, but to increase the cognitive skills involved in choosing alternatives. There is much, however, we still don't know about what works and what doesn't in substance-abuse prevention, since much of the research literature remains old and correlational. More investment in measuring what works in prevention programming, therefore, would almost certainly be fruitful. One potential line of inquiry is in the application of cognitive-behavioral-therapy techniques. Recent randomized controlled trials have shown that teaching "slow" thinking and more careful decision-making to at-risk youths can dramatically reduce criminal offending and increase school participation. Such approaches may also work for substance-use risk.
These skills-focused prevention programs may be at odds with current funding approaches. The Stanford-Lancet Commission on the North American Opioid Crisis, for instance, has called for greater integration of primary prevention services. "[P]eople who work in alcohol prevention sometimes see themselves as doing something fundamentally different from those who work in bullying prevention," the commission notes in its 2022 report. "However, the benefits to children of making substance use only one focus among many targeted by prevention efforts more than justifies the dissolution of such bureaucratic boundaries and the creation of horizontal prevention funding streams." Policymakers should be wary of mission creep in the prevention space. That said, providing funding to skills-focused programs regardless of the specific substance targeted appears likely to yield a more substantial impact.
One widely cited example of successful prevention is the nationwide "Youth in Iceland" program, which has been credited with a dramatic reduction in teen drinking and substance use in that country. The program involves an all-of-society effort, including regular survey surveillance, a national curfew for 13- to 16-year-olds, state funding for extracurricular activities as a substitute for situations that lead to alcohol and drug use, and parent contracts to encourage their involvement. As of 2020, the Stanford-Lancet Commission noted, municipalities across 32 countries are implementing the Youth in Iceland model. In the United States, expanded funding for primary prevention should include pilot programming to experiment with the Icelandic model across municipalities.
Like treatment, prevention is hard. Unlike treatment, there is nothing as effective or well-studied in prevention as the MAT buprenorphine. Per dollar spent, it is still arguably the best tool we have for discouraging marginal users. And relative to other policy areas, it is dramatically underfunded, suggesting we are leaving benefits on the table.
NOW MORE THAN EVER
Most scholars of the issue agree that drug use moves in cycles. A new drug emerges. People try it. They experience its highs, and it grows in popularity. Then problem use begins to emerge, begetting addiction, pathology, and death. Finally, the next generation of would-be users sees these side effects and tries something else to get a high. As with fashion, so with drugs — whatever the last generation did, the next generation tends to abhor.
Few people believe that policy can suppress this cycle altogether. To be sure, eliminating all drug use is not an attainable goal. But policy can almost certainly have an impact, both on the people who are currently using drugs and on the people who are considering starting. It can, in other words, flatten the cycle, making the peaks lower than they might otherwise be.
The nature of the drug crisis through which America is living now makes such efforts an urgent priority. Today's drug cycle is different from previous ones, measured not just in the number of people addicted, but the number dead. Reducing the growth of that figure, now more than ever, is a vital task for policymakers to undertake.

