Saving Medicare from Itself
At the heart of America's fiscal crisis is the looming collapse of our entitlement system. And the primary cause of that looming collapse is the explosion of costs in Medicare, the federal program that provides health insurance to every American over 65. Without major reforms of the program, there is simply no way for us to address the federal deficit, contain the national debt, or save Medicare itself from collapse.
Medicare's woes are partly demographic. In 2030, when the last of the Baby Boomers retires, there will be 77 million people on Medicare, up from 47 million today. But there will be fewer working people funding the benefits of this much larger retiree population: In 2030, there will be 2.3 workers per retiree, compared to 3.4 today and about 4 when the program was created.
But a bigger part of Medicare's troubles is the rapid inflation of health-care costs. In 2010, the per capita cost of providing health-care services in America increased by 6.1%, according to Standard & Poor's, while overall inflation increased by only 1.5%. Over the past decade, health-care inflation has risen 48%, while inflation in the broader economy has increased by only 26%, according to the Department of Labor.
Providing an increasingly expensive service to a rapidly growing population while drawing on a fast-declining pool of taxpayers is, of course, a recipe for fiscal doom. The Congressional Budget Office now projects that the Medicare program will be effectively bankrupt in 2021, and its continuing growth will increasingly burden the federal budget, sinking the nation deeper into debt. The program's trustees report that its unfunded long-term liability — the gap between the benefits that will need to be paid out and the revenues available to pay for them over the coming decades — is more than $30 trillion.
It is simply not possible to address this problem only by increasing the taxes that fund Medicare. Medicare spending is growing at a much faster rate than the economy (and therefore faster than the tax base). As Andrew Rettenmaier and Thomas Saving have shown, Medicare payroll taxes would need to quadruple today in order to cover the program's unfunded liabilities; alternatively, income-tax rates would need to increase by 57%. And even this would be sufficient only if we made the generous, but dubious, assumption that dramatic tax increases would not retard future economic growth (and thereby future tax revenues).
Another solution must be found, and soon. If Washington fixes Medicare only after a debt-driven economic disruption, the likely outcome will involve draconian across-the-board cuts in benefits to retirees, painful rationing of medical services, and restricted access to doctors and hospitals. In such a scenario, the wealthy will be affected the least, as they will be the ones most able to purchase supplemental insurance to address their needs. It will be the poorest, and the sickest, of Medicare's enrollees who will get left behind.
If Medicare reform is urgent for the sake of our most vulnerable retirees, it is also necessary for the sake of our health-care system. By subsidizing the massive over-utilization of health-care resources, and by underpaying doctors and physicians (who must pass on the costs to patients with private insurance), Medicare drives up the cost of health care not only for the elderly but for everyone. Rising costs, in turn, make health care unaffordable for tens of millions of middle-class Americans. And these problems will only get worse as the elderly become a larger share of the population.
An effective reform of the program would have to both restructure the way Medicare itself works and help to restrain the growth of health-care costs more generally. That seems like a monumental task, but ironically the poor design of Medicare actually makes that task more achievable, by making the key problems with the program readily apparent and addressable.
Legislators have understandably been reluctant to take on the task of reform, given that Medicare is popular with its recipients and that those recipients are a large and powerful constituency. But if Medicare reforms seem politically difficult now, they will be nearly impossible when the elderly population reaches 80 million. We can be certain that the retirees of the future, too, will vote in large numbers.
The time to take up meaningful Medicare reform must therefore be now. By considering the history and design of the program, as well as the reasons why past efforts to fix it have failed, we can better see our way toward a politically plausible and economically sustainable set of solutions.
WHAT IS MEDICARE?
We Americans have lived with Medicare for 45 years, so such a program may seem to us a standard component of modern government. But it is worth remembering that ours is the only developed country that makes age-based distinctions in its provision of government health coverage.
In many other countries, state-funded health insurance began with the poor, and was gradually extended up the income ladder. But in mid-20th-century America, there was still a significant stigma attached to being "on the dole," and income tests were considered demeaning.
Policymakers who sought an expanded role for government in health care thus believed that starting with the elderly would be more politically palatable. After all, the elderly were a far more sympathetic group in the public's eyes: Older Americans had less opportunity to earn their own money in order to fund their health care, and were therefore generally poorer than other Americans (along with being less healthy). Being both relatively poor and relatively unhealthy, they were in turn also less likely to have health insurance. And policymakers believed that the model of Social Security as a "self-financed" program for the elderly, paid for with a dedicated payroll tax, could easily be extended to health insurance.
For many years, however, federal health-care initiatives were successfully opposed by a coalition of Republicans and conservative Democrats, as well as by the organized force of American doctors, who feared that socialized medicine would restrict their freedom to serve their patients as they thought best. But this dynamic shifted dramatically in 1964, when Barry Goldwater challenged Lyndon Johnson for the presidency.
The 1964 election, which many on the right fondly recall as the dawn of modern conservatism, was in fact the greatest victory for the left in American history. Democrats gained 36 seats in the House of Representatives — giving them an astonishing 155-seat majority — and increased their already huge Senate majority by two seats, nudging them up to a 36-seat majority. (By comparison, the substantial Democratic majorities held after the 2008 election were merely 79 seats in the House and 20 seats in the Senate.) Even taking conservative-leaning Democrats into account, liberals were utterly in control of Washington in 1965. Suddenly, Democrats found themselves with a mandate to enact far-reaching reforms, and they did not waste the opportunity.
The very first bill of the 1965 congressional session — H.R. 1 in the House and S 1 in the Senate — was titled "Hospital Insurance for the Aged through Social Security." The focus on hospital insurance reflected the fact that hospitalization costs represented the greatest financial burden on the elderly at the time. As the so-called "Medi-care" bill zipped through Congress, Republican leaders, still reeling and disoriented from their painful defeat, criticized the proposal from the left, arguing that the legislation was inadequate because it covered neither physician services nor prescription drugs.
They proposed instead a more comprehensive but voluntary plan, comparable to the one that was at the time administered by Aetna for federal employees. But Democrats were perfectly happy to accommodate these objections within their more ambitious non-voluntary program, and the final bill included a new entitlement composed of two Medicare programs for the elderly — Part A and Part B — along with a separate health-care entitlement for the poor called Medicaid.
Medicare Part A covered hospital expenses — 60 days of hospital care after the beneficiary paid a deductible of $40 and an additional 30 days of hospital expenses for which the beneficiary would pay $10 per day. The program would be financed through a payroll tax similar to the one that paid for Social Security, though at a lower rate — a flat rate that was originally 0.7%, half of which was paid by the employee and half by the employer. Part B provided coverage for outpatient physician and nursing services, outpatient diagnostic services, medical equipment, and drugs administered by physicians (but not prescription drugs purchased by the patient). Unlike Part A, Part B would be funded by premiums from retirees, along with federal subsidies equal to those premiums.
These two parts of Medicare still constitute the bulk of the program today, and they have not changed all that much — though the deductibles have of course grown with inflation. This year, Part A covers 60 days of hospital care with a total deductible of $1,132, an additional 30 days with a deductible of $283 per day, 60 more days at $566 per day, and then all costs beyond that period. These figures would suggest some significant cost-sharing after the first two months in a hospital, but, as we shall see, the great majority of seniors have private supplemental insurance coverage that leaves them with essentially no deductible costs for Medicare at all. The payroll tax that still funds this program is now 2.9% — still shared equally between employer and employee — though the health-care law enacted last year stands to increase the employee share for wealthier workers (those earning over $200,000) by a further 0.9% starting in 2013.
Part B is also much as it was at the outset, covering physician services, outpatient care, and medical equipment. Seniors today pay a $162 deductible for such services, in addition to 20% of all costs beyond the deductible for most services — though again, supplemental insurance often covers that amount for them. In 1982, a third component was added — which came to be known as Medicare Part C, and later Medicare Advantage — under which seniors have the option of allowing private insurers to manage their Part A and Part B benefits (as discussed below). And in 2003, President George W. Bush and Congress added a prescription-drug benefit, known as Medicare Part D, in which seniors choose from a menu of approved private coverage options for drugs. Parts A and B of the program, however, remain by far its most significant and most expensive components (accounting for roughly 90% of its costs), and are the keys to Medicare's fiscal woes.
The cost overruns started very early, and were in large part an unintended function of Medicare's original design. The fact that Part B included coverage of physician services outside of hospitals meant that the great bulk of American doctors would come to interact with this new federal program — since older Americans are the ones who most frequently visit most doctors. In an effort to avoid a fight with the American Medical Association over this transformation in the lives of the nation's physicians, Medicare's designers opted not to specify any particular limits on physician-reimbursement rates. Instead, the legislation stated that doctors were to be paid according to so-called "usual, customary, and reasonable" rates — a vague reference to a system of determining payment rates that a few Blue Shield plans had been trying out in the 1960s.
The law provided no specific definition of "usual, customary, and reasonable," and essentially no guidance regarding how such a definition should be arrived at by Medicare's administrators. Medicare would pay health-care providers on a per-service basis — creating a major incentive to provide more services to patients in order to tap into this massive new source of funds — and the fee per service was left largely undefined. The program was thus launched with no clear plan for keeping its costs under control, and it included no real incentives for doctors, patients, or administrators to do so themselves.
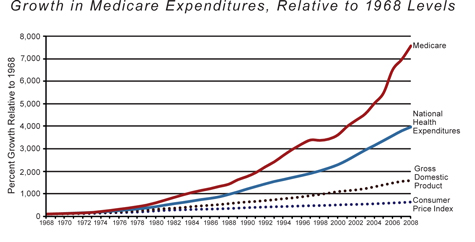
The consequences were immediate and dramatic. The annual growth of physician fees in America went from 3.8% in 1965 to 7.8% in 1966. In that same first year of Medicare's existence, hospital costs increased by 21.9%; over the subsequent five years, they grew by an average of 14% each year. These figures flummoxed government forecasters, who had projected that growth in hospital costs would actually slow after the enactment of Medicare. Instead, costs continued to grow rapidly. When Medicare was enacted, the staff of the House Ways and Means Committee (which was responsible for estimating the program's costs and effects, since the Congressional Budget Office had yet to be created) projected that its cost would grow from under $5 billion in its first year to $12 billion in 1990 — accounting for inflation — because they expected that hospital-cost growth would not exceed wage growth from 1975 onward. Instead, Medicare expenditures grew at roughly 2.4 times the rate of inflation over that period, and in 1990 reached not $12 billion but $110 billion. By 2000, the program cost $219 billion. Last year, it cost just over $520 billion. According to the Congressional Budget Office, if Medicare is not reformed, by 2020 it will cost about a trillion dollars a year.
Health-care costs beyond Medicare have also exploded in this period, and without question that has helped to drive Medicare's growth. But Medicare spending has increased faster than overall inflation in the health sector, and appears in many respects to have driven that inflation.
So what happened? Why have Medicare's costs gotten so out of control?
PUSHING COSTS UP
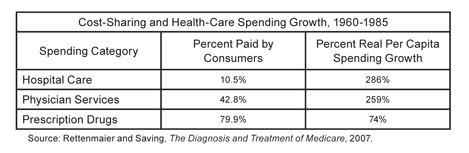
The largest driver of Medicare cost inflation is the fact that retirees bear little of the expense for their own care. As a result, seniors have no incentive to avoid unnecessary or overpriced treatments. Rettenmaier and Saving have shown that, between 1960 and 1985, growth in health expenditures was highest in those categories of spending in which consumer cost-sharing was lowest (such as hospital care), and lowest where consumers were most responsible for their own expenses (like prescription drugs, which were not covered by Medicare during that period).
The same holds true for all consumers of health care — not just the elderly. Medicaid and the system of employer-based health insurance both provide a great deal of first-dollar insurance coverage, meaning that consumers do not pay directly for services they receive and therefore have no clear sense of relative costs and values. In 1960, individuals paid directly for 52% of national health expenditures, but by 2008 that share had declined to just 12%. Americans are shielded from the real costs of their health care; as a result, it costs too much.
In theory, Medicare does include some cost-sharing provisions, especially for physician payments under Part B. But over time, private insurance companies began to realize that Medicare's design allowed them to provide seniors with supplemental coverage to pay for the deductible and co-insurance requirements of the program — a good deal for insurers (for whom costs are finite and low), as well as for the seniors who purchase such plans (and are thereby freed from any direct cost for health care). Today, almost 90% of seniors have supplemental coverage plans, which means in effect that they have unlimited health coverage for a low and fixed cost, and thereby every incentive to seek generous, and even unneeded, care.
Combined with the fact that Medicare generally pays health-care providers on a per-service basis rather than on a per-patient or per-outcome basis, this means that Medicare creates an enormous incentive for everyone involved to provide more services to seniors. Volume, more than the cost of individual services, has been Medicare's fiscal downfall. And, as discussed below, reformers trying to fix the program's finances — from the 1970s through the health-care bill enacted last year — have sought to do so through price controls that reduce the amount the program pays for each service provided, which actually creates an even greater incentive for physicians and hospitals to provide a greater number of services to make up the lost revenue.
In a detailed study of this phenomenon conducted in 2007, the Congressional Budget Office found that, between 1997 and 2005, the fees paid by Medicare for individual physician services actually declined by 5%, but the total amount spent on such services by the program increased by an astonishing 35% — because of enormous growth in volume.
Beyond the skewed incentives it creates, Medicare also inflates costs as a result of its byzantine structure, which hampers efficiency. Many people wrongly believe that Medicare is more efficient than private insurance; that view was often stated by champions of Obamacare during the debate preceding the law's enactment. These advocates argued that Medicare's administrative costs — the money it spends on expenses other than patient care — are just 3% of total costs, compared to 15% to 20% in the case of private, employer-sponsored insurance. But these figures are highly misleading, for several reasons.
First, other government agencies help administer the Medicare program. The Internal Revenue Service collects the taxes that fund the program; the Social Security Administration helps collect some of the premiums paid by beneficiaries (which are deducted from Social Security checks); the Department of Health and Human Services helps to manage accounting, auditing, and fraud issues and pays for marketing costs, building costs, and more. Private insurers obviously don't have this kind of outside or off-budget help. Medicare's administration is also tax-exempt, whereas insurers must pay state excise taxes on the premiums they charge; the tax is counted as an administrative cost. In addition, Medicare's massive size leads to economies of scale that private insurers could also achieve, if not exceed, were they equally large.
But most important, because Medicare patients are older, they are substantially sicker than the average insured patient — driving up the denominator of such calculations significantly. For example: If two patients cost $30 each to manage, but the first requires $100 of health expenditures and the second, much sicker patient requires $1,000, the first patient's insurance will have an administrative-cost ratio of 30%, but the second's will have a ratio of only 3%. This hardly means the second patient's insurance is more efficient — administratively, the patients are identical. Instead, the more favorable figure is produced by the second patient's more severe illness.
A more accurate measure of overhead would therefore be the administrative costs per patient, rather than per dollar of medical expenses. And by that measure, even with all the administrative advantages Medicare has over private coverage, the program's administrative costs are actually significantly higher than those of private insurers. In 2005, for example, private insurers spent $453 per beneficiary on administrative costs, compared to $509 for Medicare.
Medicare's fragmentary, piecemeal character leads to other problems as well. The static nature of government benefits means that Medicare remains largely stuck in the health-care models of 1965, even though considerable innovation in health insurance has taken place since then. For instance, retirees pay almost nothing for inpatient hospitalization costs in the first two months, but do pay more for outpatient physician care. As a result, the elderly have an incentive to seek expensive hospital care when less expensive outpatient care might suffice. By law, traditional Medicare is not allowed to steer patients to more cost-efficient hospitals and doctors, the way private plans can.
As already noted, repeated attempts at reducing the growth of Medicare spending have taken the form of price controls to restrict fees paid for individual services. These controls, by paying relatively more for certain diagnoses than for others, incentivize doctors to game the system instead of providing optimal care. Overall, Medicare pays doctors and hospitals about 80% of what they receive from private insurers; many providers overcharge younger patients with private insurance in order to make up the difference.
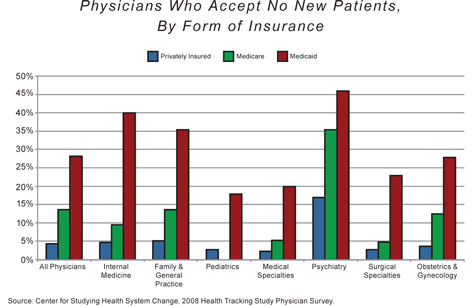
As a result of such price controls and of the program's tangled web of rules and requirements, doctors are increasingly dropping out of the Medicare program. According to a 2008 survey from the Center for Studying Health System Change, more than one-quarter of all physicians actively restrict the number of Medicare patients in their practices. The American Academy of Family Physicians says that 13% of its members did not accept Medicare patients at all in 2009 — up from 8% in 2008 and 6% in 2004.
If Medicare continues to cut physician reimbursements without fundamental reform, it will become even more difficult for retirees to find doctors who will see them. This problem has been apparent for years in the Medicaid program, which restricts physician payments even more severely than Medicare in most states. Studies show that many Medicaid patients fare worse in terms of basic health outcomes than those with no insurance at all. But thanks to last year's health-care law, Medicare payment rates are set to fall below those of Medicaid in the latter part of this decade, according to Medicare's chief actuary, Richard Foster. Unless the program is reformed to rely less on such price controls, Medicare patients will find it increasingly difficult to get care.
Without a doubt, the growth of the retiree population is also an important source of stress on Medicare's finances. That growth is driven by two factors: the aging of the Baby Boomers, and increasing life expectancy. When Medicare was enacted in 1965, the average life expectancy at birth was 70.2 years. In other words, it was anticipated that Medicare would cover an average person's health expenditures for the last 5.2 years of his life. In 2010, the average American lived to the age of 78.4; Medicare thus covered the last 13.4 years of his life — a 158% increase in the coverage period. The U.S. Census Bureau projects that, in the coming decades, American life expectancy will continue to elongate by approximately one year for every eight years that pass.
Of course, unlike the growth of costs due to the incentive structure of Medicare, the extension of life expectancies is not bad news. The overall story of Medicare is not entirely bad, either. The program has provided the elderly with health insurance for more than four decades. Seniors rely on it and like it; the program is extremely popular. But along the way, it has done grave damage to our broader health-care sector — contributing to an unsustainable inflation of costs that puts the program itself in jeopardy, and that makes it harder for younger Americans to afford insurance for themselves and their families.
Today, the program's finances are completely out of control. And the illusion of pre-funded benefits — the notion that Americans pay into the system while they work and then merely withdraw the funds they put in when they retire — no longer bears any relation to reality. According to calculations published earlier this year by Eugene Steuerle and Stephanie Rennane of the Urban Institute, the average two-earner married couple retiring in 2010 had paid $109,000 in Medicare taxes while working, but will receive $343,000 in benefits during retirement. A similar couple retiring in 2030 will have paid $167,000 in taxes and will receive $530,000 in benefits. Medicare is simply a massive (and growing) transfer of resources from younger to older Americans. And since the elderly are no longer the poorest Americans — on the contrary; Americans over the age of 65 are now significantly wealthier than younger Americans — that often means that Medicare is a transfer of resources from poorer to wealthier Americans. The illusion of an earned benefit, like the illusion of Medicare as a self-sustaining program, must be overcome if we are to address Medicare's woes.
Clearly, it is well past time to save Medicare from itself. But how?
FAILED FIXES
Because the problem of cost overruns became apparent so soon after Medicare's enactment, almost every president after Lyndon Johnson tried his hand at restraining the program's growing expense. In 1972, under Richard Nixon, Congress allowed for the creation of Medicare health-maintenance organizations, in the hope that private managed care might help keep down the program's costs. Consumers had little incentive to use them, however, and the experiment was a failure. Nixon's other Medicare adjustment undermined his efforts: He also expanded Medicare to include people under 65 who qualified for Social Security disability benefits and had received them for two years, which of course only further swelled Medicare's budget.
In 1977, under Jimmy Carter, the Health Care Financing Administration was created to more efficiently administer Medicare and Medicaid, setting the programs apart from Social Security. In 1983, under Ronald Reagan, HCFA imposed a "prospective payment system" whereby hospitals and physicians would be reimbursed at a set rate for a specific diagnosis — Medicare's first price controls.
But after a few years, hospitals and physicians grew wise to the new system, and found ways to shift patients from poorly paying "diagnosis-related groups" to higher-paying ones — a practice called "upcoding." So in 1988, a team led by William Hsiao, an economist at the Harvard School of Public Health, proposed a new system of price controls for Medicare called the Resource-Based Relative Value Scale, or RBRVS. Hsiao invented a complex formula that combined the time, effort, judgment, skill, and stress of addressing a specific medical problem (the "physician work" factor) with local medical-practice costs and related considerations. The formula was adopted by Congress as part of the 1989 budget deal in an effort to manage Medicare's costs. But few of Hsiao's factors had anything to do with the way in which economies normally price goods and services, and the RBRVS system did little to improve the economic value of health-care decisions, or Medicare's finances.
Also in 1988, Congress passed the short-lived Medicare Catastrophic Coverage Act, which expanded Medicare Part A to cover an unlimited number of hospital days, eliminated the daily co-insurance requirement for stays longer than 30 days, and provided a benefit for outpatient prescription drugs, among numerous other perks. President Reagan had insisted that the MCCA be deficit-neutral; it therefore incorporated a means-tested supplemental premium of up to $800 to pay for these extra benefits. But that supplemental premium proved to be extremely unpopular with retirees, and the entire law was repealed in 1989.
The next major push for Medicare reform began in the mid-1990s. The new Republican Congress proposed reducing projected Medicare spending by $270 billion, along with a package of tax cuts; President Clinton accused Republicans of fleecing Medicare to aid the wealthy, and counter-proposed $128 billion in reductions with no tax cuts.
Eventually, in 1997, the two sides produced the Balanced Budget Act, which included an important Medicare reform. The law created the Sustainable Growth Rate, a formula that tied physician reimbursements to GDP growth as a way of keeping costs under control. While the SGR may have helped to hold down costs in the short term — Medicare expenditures were essentially flat in 1998 and '99 — by 2001, those costs had resumed their historical growth rate. The 1997 law would thus have required significant cuts in doctor fees, but doctors protested, and Congress began passing so-called "doc fix" legislation to increase physician reimbursements above their SGR-mandated levels — essentially ignoring the law's requirement on an annual basis almost every year since 2003. As a result of politics and interest-group concerns (not to mention the basic economics of health care), price controls have thus proven a thoroughly inadequate means of holding down Medicare costs.
Unfortunately, Obamacare only doubles down on this failed approach. Like prior attempts to limit costs through price controls, the new law simply caps annual Medicare growth but fails to fundamentally transform the system to allow it to live within such caps. Starting in 2015, per capita Medicare spending growth will be limited to a fixed rate set between the general rate of inflation and health-care-cost inflation. Then, starting in 2018, that rate will be set permanently at per capita GDP growth plus one percentage point — a rate far lower than Medicare's growth in recent decades. And just how will costs be kept within these boundaries? The law establishes a board of experts — the 15-member Independent Payment Advisory Board — that will be charged with making the necessary changes to Medicare's payment rates and practices. But the board is prohibited from requiring greater cost-sharing by Medicare recipients, and from changing the basic "fee-for-service" structure of the program. So it cannot pursue market-based reforms. All it can do is tweak the program's price controls, in the hope that just the right mix of cuts in payments to doctors and hospitals will cause those doctors and hospitals to become more efficient.
This is exactly the approach that has failed to control prices in the past, and the one that Congress has had to override each year through the "doc fix." It simply pays doctors less and less for the same services without giving them any incentive to improve their efficiency or productivity by changing how they work. There is no reason to imagine this oft-failed approach will succeed this time around. Indeed, in May, the Medicare program's own actuary explained why he expects Obamacare's price controls to fail:
By the end of the long-range projection period, Medicare prices for hospital, skilled nursing facility, home health, hospice, ambulatory surgical center, diagnostic laboratory, and many other services [under the new law] would be less than half of their level under the prior law. Medicare prices would be considerably below the current relative level of Medicaid prices, which have already led to access problems for Medicaid enrollees, and far below the levels paid by private health insurance. Well before that point, Congress would have to intervene to prevent the withdrawal of providers from the Medicare market and the severe problems with beneficiary access to care that would result. Overriding the productivity adjustments, as Congress has done repeatedly in the case of physician payment rates, would lead to far higher costs for Medicare in the long range than those projected under current law.
Medicare's future under Obamacare thus looks much like its past — only worse.
MARKET REFORMS
But if price controls have been a failure, most attempts at market-oriented reforms have not fared much better. In 1982, Congress introduced Medicare Part C, which allows private insurers to administer Medicare plans at 95% of the combined cost of Part A and Part B. The idea was that these private plans could save money because they would integrate Part A and Part B coverage into a single benefit package, and would thus be managed more efficiently by private entities. Part C was popular with retirees; enrollment grew at 30% a year in the mid-1990s, peaking at 16% of Medicare enrollees in 1999. But unfortunately, this system strongly incentivized private plans to "cherry-pick" younger and healthier retirees, leaving the rest to traditional Medicare — thereby raising, rather than reducing, overall costs (because the larger traditional Medicare program still dominated the health-care market, and so its higher costs meant higher health-care costs overall).
Things changed in 1997, when the Balanced Budget Act introduced a more sophisticated risk-adjustment system so as to curtail cherry-picking. As a result, insurers started to drop out of Part C (since their costs were going to rise), and enrollment stalled. It turned out that, for beneficiaries of equivalent health and age, private plans were slightly more costly than traditional Medicare, because the fragmented community of private insurers lacked the government's market power to negotiate lower rates. The fact that private insurers had to compete in the same market with traditional Medicare put them at an immense disadvantage, yet Medicare's market advantage did not make it any more efficient or cost-effective.
This problem was revisited in 2003, when President Bush signed the Medicare Modernization Act. The MMA increased reimbursements to private insurers in order to compensate for their lack of market power; by 2009, Part C plans (rechristened "Medicare Advantage" plans) were paid 14% more per patient on average than traditional Medicare. In return, private insurers reduced premiums. These changes increased the popularity of privately-managed Medicare plans; by 2010, Medicare Advantage enrolled 11 million retirees, or nearly 25% of all Medicare participants. But again, they did not significantly reduce costs, as they were still playing in a field dominated by a highly inefficient fee-for-service Medicare program.
Market-based reforms cannot have their desired effect — introducing meaningful competition and consumer pressures to bring down costs — as long as this traditional fee-for-service structure of Medicare remains the dominant force in the market, because providers still have a powerful incentive to conform their behavior to Medicare's inefficient design. For a market reform to work, it seems, it has to be comprehensive — either replacing traditional Medicare or turning it into just one option among many. Today's reformers would be wise to keep this lesson in mind.
The most successful cost-control experiment in Medicare — the relatively new prescription-drug component called Part D — has been proving this point. The Part D benefit, added in 2003, is a so-called "premium support" program. Seniors are given a set amount of money to apply toward their choice of plan, selected from a menu of private prescription-drug coverage options. If they prefer a more expensive plan, they can make up the difference themselves. Because this premium-support program is the only source of prescription-drug funding in Medicare, it is able to bring real market forces to bear.
The program also contains a further cost-control mechanism that has come to be known as the "donut hole," by which recipients are required to pay for all drug costs above a certain minimum level and below a ceiling — a design intended to simultaneously make seniors sensitive to prices yet shield them from catastrophic costs. In 2009, the donut hole required retirees to pay 100% of prescription-drug costs above $2,700 and below $6,154, in order to discourage unnecessary spending. (Obamacare would eliminate this element of the program as well — sparing seniors from the donut hole, but thereby also shielding them from market forces that can help restrain costs.)
These two market-based elements have indeed kept costs down for this component of Medicare. While Medicare Part D has provided drug coverage to most Medicare recipients and is very popular with seniors, it has so far come in more than 30% below the original cost expectations of the Congressional Budget Office. In a recent report, the actuary of Medicare projects that Part D's cost over its first decade will likely be more than 40% below those original estimates.
Some market-based reforms, then, can work. The premium-support model of Medicare Part D has been a great success. But its application has been limited, and overall Medicare costs continue to climb.
PREMIUM SUPPORT
Could there be a way to apply the lessons of this "premium support" and cost-sharing approach to the broader program? The history of failed reform efforts includes one intriguing twist that suggests there just might be.
In 1997, as a result of the Balanced Budget Act, Congress organized the National Bipartisan Commission on the Future of Medicare, under the leadership of Democratic senator John Breaux and Republican representative Bill Thomas. The commission's final recommendation, supported by members of both parties, was that Medicare should be converted to a "market-based Premium Support model" similar to the one used in the Federal Employees Health Benefits Program.
Under the commission's proposed system, retirees would have been able to choose between private health plans and a traditional government-run fee-for-service plan (a consolidation of Medicare Parts A, B, and C). Thus traditional Medicare would have become one option among many, competing for business. Regardless of what option they chose, beneficiaries would have been expected to pay a premium equal to 12% of per capita health costs, but would have paid no premium at all if they bought a plan that was at least 15% cheaper than the average one. In addition, the commission recommended increasing the Medicare eligibility age from 65 to 67, in harmony with Social Security.
After the commission made its proposal, President Clinton made a counter-proposal, shaped in large part by his Treasury secretary, Lawrence Summers. He proposed "managed competition" for Medicare, in which private insurers would have engaged in competitive bidding for health coverage of the elderly. Retirees who chose plans that cost less than the average bid would have retained three-fourths of the savings. Clinton also proposed new subsidies to encourage employers to retain private-sector health coverage for their retirees, taking some of the burden off of Medicare.
These two sets of proposals were, in many ways, quite compatible. Indeed, according to historian Steven Gillon, President Clinton and House Speaker Newt Gingrich, along with several prominent Senate Democrats, were close in 1997 to a historic agreement for reforming Medicare along these lines. But after the Monica Lewinsky scandal erupted in early 1998, Clinton was focused on defending himself from impeachment, and this required currying the favor of ideological Democrats over pragmatic ones. Thus no serious effort was made to bridge the various reform proposals, and Medicare's problems went unresolved.
Even though it went by the wayside, the basic structure of the Breaux-Thomas commission's proposal — transforming Medicare into a premium-support system in which retirees have a pre-set benefit they can use toward the purchase of approved private insurance plans — remains the most plausible approach to addressing Medicare's immense and growing problems. A number of reform proposals offered in the years since the commission's report have followed its lead in general terms, though always with particular tweaks or additions.
The most prominent, and surely the most important, of these is the 2012 budget resolution recently passed (by the Republican majority on a party-line vote) in the House of Representatives. Proposed by House Budget Committee chairman Paul Ryan, the budget included a plan to transform Medicare into a premium-support system beginning in 2022. This would mean that all current retirees, as well as people who will retire by that year, would be left in the existing Medicare system (unless he chooses to, no American now over the age of 55 would be transitioned into the system of premium support); a new structure, however, would be established for new retirees from 2022 onward.
Rather than pay all providers a set fee directly, this approach would let retirees use the money (in the form of a premium-support payment that would start at current Medicare rates and grow with overall inflation) to choose insurance plans from a menu of private coverage options. To participate, private insurers would have to agree to accept all Medicare recipients, to charge the same premiums to all beneficiaries of the same age, and to provide at least a minimum benefits package required by the Office of Personnel Management (which runs the Federal Employee Health Benefit Plan), with the idea of providing all seniors with guaranteed affordable comprehensive coverage.
The level of premium support would increase with age, and poor seniors and those in the worst health would also get significantly greater support, while the wealthiest would receive less and so need to use more of their own money to buy coverage. And the premium-support model would not be a small experiment overshadowed by traditional Medicare (and thus unable to really change the way insurers and providers do business): It would be the core of the new Medicare system, and the means by which seniors would be guaranteed coverage.
This approach, then, would work like the Medicare prescription-drug benefit (and like the health-insurance program made available to federal employees). Insurers and providers would need to compete for seniors' dollars, and to do so they would be free to find innovative ways to offer better quality at lower costs. That's how markets produce efficiency: by letting sellers find ways to offer buyers what they want at prices they are willing to pay.
Although the precise effect of this approach on overall health-care costs is difficult to predict, there is no question that such a reform would dramatically improve Medicare's fiscal prospects and reduce the burdens it would place on the broader federal budget.
FIXING MEDICARE
Something like the Ryan approach will be crucial to the future of Medicare. The program is set to go bankrupt in a decade, and seems past the point of small fixes or yet another tweak to the price-control formula (as proposed under Obamacare). A broader reform must come. Medicare's history, its importance to the seniors who depend on it, and the nature of its fiscal problems suggest that such a reform must take account of six factors.
First, we must remember that Medicare's primary achievement — protecting economically vulnerable retirees — is a salutary one, the preservation of which must be the cornerstone of reform. We must also promise current and soon-to-be retirees that their benefits will not change. As many have suggested (and as the Ryan budget proposes), reforms should be implemented only for future enrollees age 55 or younger, in order to allow for a gradual transition into a reformed system, and to preserve benefits for those who have long planned their retirements around the existing system.
Second, we must appreciate the power of cost-sharing. When patients are aware of the costs of their care, and assume partial responsibility for higher expenditures, they are more likely to make sensible decisions about whether to pursue treatment. This can do much more to curb health-care cost inflation than can crude price controls or benefit cuts. As discussed above, from 2003 to 2010, Medicare's prescription-drug benefit contained significant cost-sharing provisions, in plans administered entirely by private insurers, and the program came in under budget as a result. Most important, so long as Medicare remains in its current form, the role of supplemental "Medigap" plans must be seriously re-examined. These plans do much to undermine value-oriented health-care consumption by shielding seniors from all cost-sharing.
Third, we must introduce means-testing into Medicare. Some conservatives, because of their aversion to wealth redistribution, have opposed means tests; some liberals have opposed them because they fear that Medicare will lose political support if its benefits are not uniform. Both of these arguments fail to stand up to scrutiny. If we raise taxes to bridge our enormous deficits instead of reducing Medicare spending, those taxes will fall disproportionately on the wealthy and discourage economic growth. Spending less is a better solution, because taxes cannot be increased as quickly as Medicare expenditures will rise. As to Medicare's political support, the explosive growth of Medicaid shows that welfare programs can have just as much support as entitlements do. Either way, the political concerns of the left and right pale in comparison to the fiscal crisis we now face.
Fourth, we should index the Medicare retirement age to life expectancy, as tabulated by the Census Bureau each year. This would ensure that the program is not exposed to increases — expected or unexpected — in American longevity. Once again, the Bipartisan Medicare Commission of the late 1990s offered a framework for thinking about how to adjust the eligibility age for Medicare. Improving our age-dependency ratio — the number of retirees per worker — must come in part through normalizing our retirement age, inducing more middle-aged people to remain in the work force, and from restoring the tax subsidies (eliminated by Obamacare) that encourage employers to maintain private health coverage for retirees.
Fifth, we must address the substantial problem of Medicare fraud. It is estimated that $60 to $100 billion of annual Medicare spending — between 8% and 13% of the total — is fraudulent. Medicare processes over one billion claims per year, and is required by law to reimburse claims within 15 to 30 days. This makes it almost impossible to prevent criminal activity. Private administration of the program would do much to incentivize the development of more thorough auditing practices.
Finally, Medicare must evolve into a system in which individuals can shop for value in insurance plans. They already have the ability to do this with Medicare Parts C and D, but not with A and B. As discussed above, the Breaux-Thomas commission proposed a premium-support system in which Medicare would subsidize retirees in purchasing insurance. The Ryan budget suggested a similar approach, as did the deficit-reduction task force of the Bipartisan Policy Center, headed by former Republican senator Pete Domenici and former Congressional Budget Office director Alice Rivlin, a Democrat, earlier this year. Some of the specifics of their plans differed, of course, but they shared the conviction that a transition to premium support is essential to Medicare's future.
MEDICARE IN CONTEXT
Important as these reforms of the structure of Medicare would be, an enduring solution to Medicare's problems would also require a reform of the broader health-care system.
Until our whole system moves in the direction of an individual market for health insurance, we will have no voluntary mechanism by which to encourage Americans to shop for value in health care. If overall health spending for Americans below the age of 65 continues to rise at a much faster pace than inflation (because of the perverse incentives of the employer-based insurance system and of Medicaid), Medicare's expenditures will rise with it.
Addressing this problem would require reforming and integrating Medicare, Medicaid, the employer-sponsored system, and the individual market (and would therefore require replacing Obamacare with a very different set of health-care reforms well beyond Medicare). It would involve addressing the runaway costs of defensive medicine and medical-malpractice litigation. Such changes would of course be extremely difficult to undertake, as the heated ongoing health-care debate amply demonstrates. But a meaningful and effective reform of Medicare could offer a plausible first step along such a path — addressing some of the most significant causes of the cost-inflation problem, and offering proof that sensible market-based reforms can work.
This moment in our politics — when our long-term fiscal situation has suddenly captured public attention — might just offer the opportunity to attempt such a step. It is an opportunity we must not allow to slip by.